Testimonial: minimizing peri-implant tissue loss
I started using this concept in its first version when it was proposed four years ago, because it was part of a digital transition logic that I was implementing in my practice. Today, this digital tool, however small, is undeniably one of the biggest revolutions in modern implantology. It's both a surgical tool, a Profile Designer to guide the healing of peri-implant soft tissues in an anatomical way, and a digital tool, a scanbody, for non-invasive and incredibly precise digital acquisition of the implant situation.
It's a three-in-one tool. It enables anatomical healing of peri-implant tissues by selecting the most appropriate shape to recreate the prosthetic emergence in line with the tooth to be reconstructed. It is also a formidably simple and precise tool for taking impressions: either by optical impression in the chair, in which case it acts as a scanbody, or by physical impression, which is subsequently digitized in the prosthetic laboratory. It's not necessary for the clinician to be equipped with an intraoral CT scan! But it is often a further incentive to invest…
In fact, the impression session, which is often resented by patients, has been greatly simplified. Users are unanimous: the duration of this session is divided by three, and it takes a considerable amount of stress off both practitioner and patient! It also facilitates exchanges between surgeons and their correspondents, increasing their complicity. Last but not least, it can also be used to support a provisional prosthesis by means of a breakaway abutment system in white Peek that clips into its screw well (a short screw, supplied with the provisional abutment, then replaces the original screw to enable indexed engagement of this retentive element). The transitional prosthesis can then simply be produced using the isomolding technique commonly used in conventional prosthetics, or can be reconstructed using CAD/CAM.
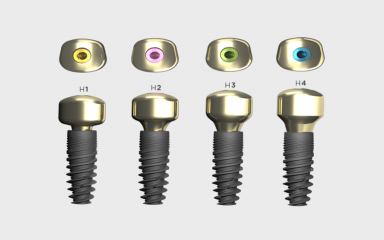
If there's one major clinical benefit to be gained from my years of experience and patient follow-up, it's tissue preservation. Each of the three features mentioned above contributes to minimizing peri-implant tissue loss. The printed prosthetic cradle enables tissue to be sculpted during the healing phase ("Shaping Profile"). The prosthesis produced after this period is perfectly adapted to the receiving bed, without creating tension on the tissues. The impression requires no manipulation of abutments or transfers. As a result, fragile scar tissues are not damaged as they could be by repeated manipulations. What's more, the digital impression technique is extremely precise.
Thanks to the positive feedback I've received on the clinical results observed, I'm now opting for a standardized protocol that can be reproduced in aesthetic clinical practice. Whenever possible, I perform the flapless extraction and implantation in the same surgical step, systematically using a single-use Iphysio healing abutment, selecting the most suitable shape to fill the gingival socket and also lining it with its FRP "pancho" covering a supply of bone particles (human bank bone) inserted into peri-implant bone gaps greater than 0.5 mm. Finally, I top these elements with an immediate provisional prosthesis (set in underbite, of course), since patients' aesthetic demands are omnipresent.